Introduction.
I would like to experience the “Interview AI,” which uses AI to immediately transcribe and automatically convert the interview into a natural interview format, with audio files of actual interviews.
The audio file to be used for this project will be a 25-minute audio interview about a physician’s career.
Upload audio file and start transcription
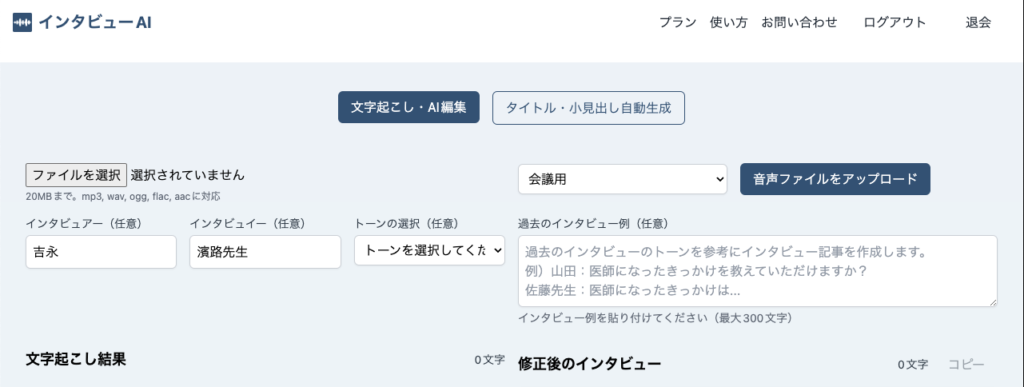
First, open the Interview AI website and log in.
Once logged in, select the audio file from the “Select File” button.
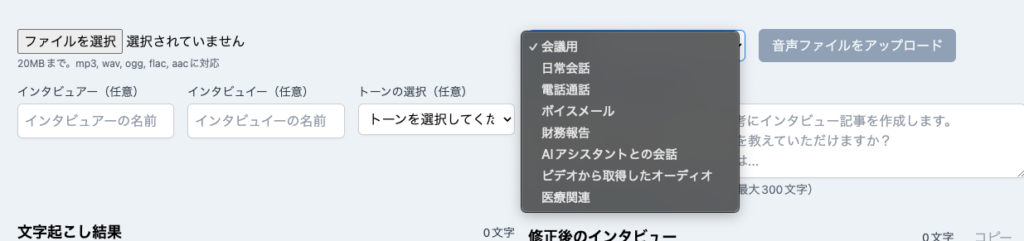
To the right of the file selection, there is a pull-down list to select the audio file type. In this case, select “For Conference”.
Also, enter “Yoshinaga” as the interviewer and “Dr. Hamaji” as the interviewee.
After completing the input, click the “Upload Audio File” button.
Transcription will begin after the audio file is uploaded.

The transcription results were finished in only 10 seconds for a 25-minute audio file, and automatic correction to conversational format began directly afterwards.

Transcription results (processing time: 10.3 seconds)
In the case of this 25-minute audio file, the transcription result was displayed in 10.3 seconds as follows.
That’s 12,142 characters in all.
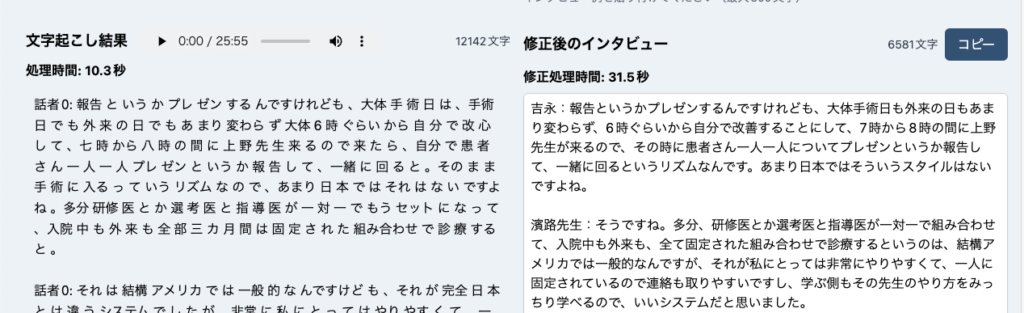
There is also speaker separation, as in “speaker 0” and “speaker 1,” but it’s not perfect.
The accuracy of the transcription does not seem to be bad, but it is not perfect, with the “one-to-one correspondence” section being “one-to-one sun”.
Speaker 0: I do a report or presentation, but generally on a surgery day, whether it is a surgery day or an outpatient day, I usually start at around 6:00 a.m. to make myself available, and when Dr. Ueno arrives between 7:00 and 8:00 p.m., I do a presentation or report on each patient and go around with him or her. The rhythm is to start the procedure as it is, which is not the case in Japan. The resident or selective doctor and supervising doctor are set up as a one-on-one team, and all patients, both inpatients and outpatients, are treated in a fixed combination for the entire three-month period.
Speaker 0: This is quite common in the U.S., but it is a completely different system from Japan, but it was very easy for me to work with.
Speaker 1: Do you have contacts with more than one fellow?
Speaker 0:. Basically one on one.
Speaker 1: . Okay, then.
Speaker 0: Many
Speaker 1: Yes. Speaker 1: Yes, and fellows. We need a lot of senior doctors. For example, one-on-one interviews are troublesome.
I can’t see the speaker 0:. There are six staff members and six residents or fellows, so it’s kind of like one-on-one sun.
Speaker 0: Once I got used to the system, I felt that the system was systematic and easy.
Speaker 1: Right. Speaker 1: Yes, that’s right. The U.S. is a country with a very good system.
Speaker 0:.
Speaker 1: In this sense, I think that the training is much easier to do than in Japan.
Speaker 0: I have an image of Japanese surgeons working all the time without a break. I have the image of Japanese surgeons working all the time without a break, but how is it in the U.S.?
Speaker 1: Well, at least for the fellows and residents, we are always on duty, so on weekends we are always on duty.
Speaker 0: Oh, it’s a complete vacation, so some people go on trips. Yes, Dr. Ueno will be the primary doctor, so it’s kind of like an accessory, like a ferro, or something. I see. I see. So you are on and off the job quite well, I guess. At least in my resident fellows, I was on and off the clock, and I was only on weekend duty about once every three weeks, so when I was on duty, I had two or three times as many patients as usual, which was a lot of work. Did you go on a fellowship as a clinical intern and stay on as a supervising physician?
Speaker 0: That’s why you can’t slow down. In order to remain as a medical advisor, you have to obtain a specialist degree, and you cannot obtain a specialist degree only as a fellow, so we have made sure that this is well taken care of. The system is designed so that fellows cannot become specialists in the program for foreigners unless they have been in the same program from the first year. Basically, many fellows from overseas return to their home countries after two or three years of training? Yes, that’s right. It is a program that they have already decided to do. Rather than staying in the U.S. for the rest of their lives, they wanted to live in the U.S. for a few more years as a training program. Yes, that’s right. I am always in the middle of a CPR calculation, so I am six years behind my peers.
Speaker 0: Of course, the U.S. was good for a quick turnaround. The number of cases is much higher than in the US.
Speaker 1: I don’t think you ever thought of pursuing a medical specialty in the U.S.
Speaker 0: Yes, I thought about it for a moment. I thought about it for a moment, but then I realized that there was a big price to pay. I thought that I would have to start over from the first year, that there was no guarantee that I would make it to the end of the program, and that I would have to completely cut off my path in Japan, which I did not think was an easy path to take.
Speaker 1: Did you have any predecessors who were doing clinical work in the U.S.? Speaker 1: Yes.
Modified interview (processing time 31.5 seconds)
Next, let’s look at the revised interview.
This one took 31.5 seconds to finish correcting the transcription result, which is 6581 characters. At this point, filler words (“ah,” “uh,” etc.) are gone.
It also shows that the interviewer (Yoshinaga in this case) and interviewee (Dr. Hamaji in this case), which were specified before transcription, are reflected as speakers. The separation of speakers was not perfect at the time of transcribing, but is now cleanly separated in the revised interview.
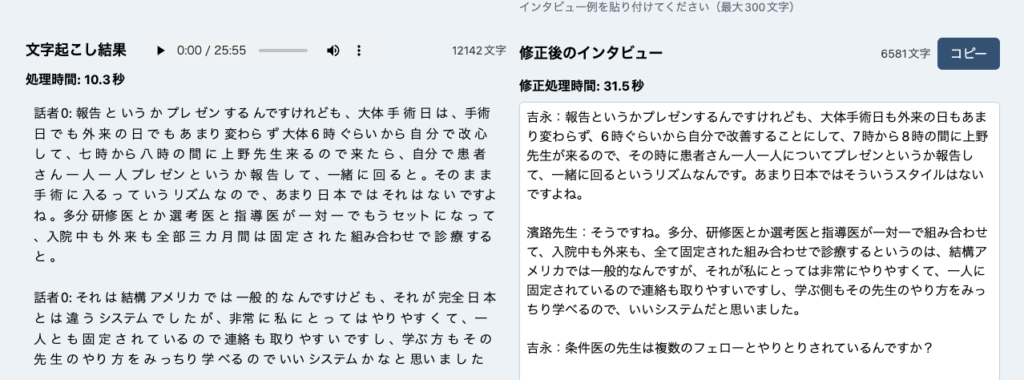
It is also clear that most of the typographical errors (e.g., one-to-one sun) that were scattered at the time of transcription have been eliminated.
Yoshinaga: I make a report or presentation, but it is generally the same on surgery days and outpatient days, and I decide to make improvements myself from around 6:00 a.m. Dr. Ueno comes between 7:00 and 8:00 a.m., so I make a presentation or report on each patient at that time and we go around together. That kind of style is not so common in Japan.
Dr. Hamaji: Yes, that’s right. It is quite common in the U.S. to have a one-on-one combination of residents, selective doctors, and supervisors, both inpatient and outpatient, all of whom are fixed in place. I thought it was a good system because it was fixed to one person, so it was easy to contact him or her, and the students could learn his or her way of doing things.
Yoshinaga: Do the condition doctors communicate with more than one fellow?
Dr. Hamaji: Basically, one-on-one.
Yoshinaga: So there are a lot of people with the condition?
Dr. Hamaji: We need a lot of fellows and a lot of senior doctors to take care of them on a one-to-one basis. For example, we have six staff members and six residents or fellows, so it is like a one-to-one rotation.
Dr. Hamaji: Once you got used to it, it was systematic and easy, or something like that.
Yoshinaga: Yes, that’s right. The United States is a country with a very good system.
Dr. Hamaji: In that sense, I think there are many aspects that are very much easier to do than in Japan as a training recipient.
Yoshinaga: I have the image of Japanese surgeons working all the time without a break, but how about in the U.S.?
Dr. Hamaji: Yes, at least for fellows and residents, we have a set duty schedule, so we are completely on duty on weekends. If I am on duty, I go to the hospital and work every day, but if I am not on duty, I am completely off from Friday night until Monday morning.
Yoshinaga: Oh, you are completely off. Do some of you go on vacation?
Dr. Hamaji: Well, I’m not a primary care physician, so Dr. Ueno will be my primary care physician, but fellows and such are ancillary.
Yoshinaga: I see. Do you feel like you are on and off quite well?
Dr. Hamaji: Yes, that’s right. At least residents and fellows have a clear on/off schedule, and weekend duty was usually only once every three weeks. If I was on duty, I would be responsible for two or three times more patients than usual, so it was tough, but if I was not on duty, I could do what I liked very much.
Yoshinaga: Did you go to clinical study abroad as a fellow and stay on as a supervisor?
Dr. Hamaji: That is not easy to do. In order to stay on as a medical advisor, you have to become a specialist, so you cannot become a specialist just by being a fellow. The system is so well designed that unless you are in a certain program from the first year, you cannot become a specialist in a program for foreigners.
Yoshinaga: Basically, do most fellows from abroad return to their home countries after two or three years of training?
Dr. Hamaji: Yes, that’s right. That is already a definite kind of program. As a teacher, do you feel that you would rather live in the U.S. for a couple of years for training once, rather than for a lifetime?
Dr. Hamaji: Yes, that’s right. In my case, I inevitably advanced to respiratory medicine in the middle of my career, so I am six years behind my peers, or rather, my age group.
Yoshinaga: Are you saying that it is difficult to get it all back at once?
Dr. Hamaji: Of course, it was good in the US. The number of cases is different, of course, because there are many more cases.
Yoshinaga: Did you always have the idea that you would like to get a medical specialty in the U.S. as well?
Dr. Hamaji: Yes, I thought about it for a moment, but considering the circumstances at the time, I thought the cost would be too great. There was the fact that I would have to start over from the first year, there was no guarantee that I would be able to go all the way through once I entered that program, and I would be completely cutting off my options in Japan, so I thought that would not be an easy path to take.
Yoshinaga: Did you have any seniors who were clinically practicing in the U.S.?
Dr. Hamaji: Yes, yes.
Dr. Hamaji: Nowadays, especially when it comes to cardiac surgery, I think there are relatively many people who are teaching in the U.S. because they are treated better in the U.S., which is very attractive in terms of job satisfaction. Conversely, cardiac surgery is not very popular over there, so there are slots available. Americans don’t really want to become a cardiothoracic surgeon, so there are openings. So the treatment is better than in Japan.
Yoshinaga: Indeed, there is no comparison, perhaps. I think you have compared medical care in Japan and the U.S. If you have any kind of good or bad points about each, please let us know.
Dr. Hamaji: Well, to put it simply, if I am on the side of providing medical care, I would like to work in the United States. If I were on the receiving end of medical care, I would want to receive it in Japan.
Yoshinaga: So is it related to the insurance system or something else?
Dr. Hamaji: Yes, the insurance system is the same, the cost factor is the same, and the quality of medical care is the same.
Yoshinaga: In terms of the respiratory surgery you went to, do you think that Japan is superior in terms of quality and surgical quality?
Dr. Hamaji: Yes, the place where I trained is probably one of the very best in the U.S., but even so, it probably does not match the quality of surgery in Japan, at least in respiratory surgery. Unfortunately.
Yoshinaga: Is it in terms of the number of cases that you would still prefer to work as a doctor in the U.S.?
Dr. Hamaji: Yes, that’s right.
Yoshinaga: What do you think about life in the U.S. and the medical environment? Especially in terms of vacations and satisfaction.
Dr. Hamaji: I am a little sensitive about vacation and satisfaction. For now, I think the U.S. is far ahead in terms of income and holidays. However, I feel that Japan is better in terms of procedures and the meticulousness of medical care. In particular, I feel more secure in Japan when it comes to the attention to detail of medical institutions. In the U.S., even if you make a small complaint, they often do not respond promptly, so aside from good and bad things, I think Japan is more attentive to various details.
Yoshinaga: I see, so there are such differences. So, do you have any advice for those who wish to study in the U.S. for a long period of time?
Dr. Hamaji: Yes, I think you should be careful if there is a possibility of receiving medical care. Nevertheless, I would like many people to experience training in the United States. Ultimately, it will help raise the level of medical care in Japan, and the main reason is that I want that person to be happy.
Yoshinaga: So working in the U.S. leads to happiness.
Dr. Hamaji: Yes, broadly speaking, you are more likely to be happy working in the US. However, if you or your family members need to receive medical care in the U.S., or if you have a chronic illness, you may want to think twice. There is a high possibility that the detailed medical care you have received in Japan will not be available in the U.S.
Yoshinaga: Thank you very much. I would like to ask you about your specific experience regarding the differences in medical care in the U.S. and Japan. Has Dr. Hamaji ever received medical care in the U.S.?
Dr. Hamaji: I haven’t received much, but I can understand the differences from what I have heard and read. Is there anything else you forgot to tell us about studying abroad?
Yoshinaga: What is special about it?
Dr. Hamaji: I can only talk about clinical study abroad, but there is also research study abroad. I believe that by studying abroad for research, you will gain a completely different experience. In the process, you will encounter different ways of thinking and different perspectives from Japanese researchers, and this is something you will definitely gain. I encourage you to go, even for a short period of time if time and money permit, regardless of whether it is clinical or research.
Yoshinaga: That is wonderful. I would like to ask you about how Dr. Hamaji is currently a professor at Nara Medical University.
Copy and share the revised interview
The modified interview can be pasted to the clipboard by clicking on the “Copy” button in the upper right corner.
You can paste it directly into your own notepad, word document, blog post, interview article, etc.

summary
In this issue, we describe the results of our experience with the “Interview AI,” which uses AI to immediately transcribe and automatically convert the interview into a natural interview format, with audio files of actual interviews.
It is good that the transcription is done quickly. Also, at the time of transcription results, there were some parts that were not perfect, such as speaker separation and typos, but almost all of them were resolved by the subsequent automatic correction function to conversational format, so it seems that the corrected interview can be used by copying it as is or partially correcting it.